No products in the cart.
by Raj Kaur Khalsa (Naila Omar Khayyam Alieva), Ph.D.
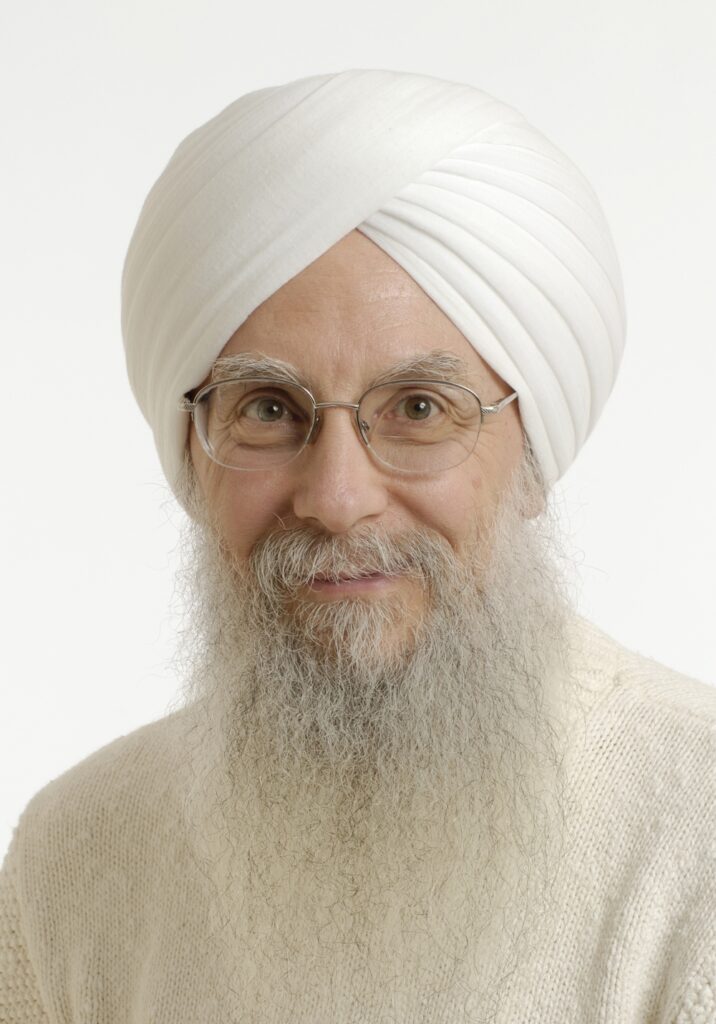
Sat Bir Singh Khalsa, Ph.D.

Inflammation is a disordered physiological response or consequence of immune reactions to acute injury or a chronic condition and has been associated with a number of diseases. Inflammation involves local or global changes in blood vessels, nerves, and tissues with symptoms including pain, redness, immobility, swelling, and heat of the affected area. Additionally, inflammation of internal organs, often associated with chronic conditions, may also occur and could include fatigue, nausea, mouth sores, chest pain, abdominal pain, fever, rash, joint pain, sleep disturbance, depressive mood, irritability, and mild cognitive difficulties with attention and memory. Chronic inflammatory diseases are the most significant cause of death in the world. The World Health Organization (WHO) ranks chronic inflammatory diseases as the greatest threat to human health. Worldwide, three of five people die due to chronic inflammatory diseases like stroke, respiratory diseases, cardiovascular disorders, cancer, obesity, and diabetes.
Inflammation is actually a defence mechanism in the body and a part of the body’s normal immune response. Infections, wounds, and any tissue damage would not be able to heal without an inflammatory response. In cases where harmful stimuli have not been removed and the inflammatory response has been maintained for a long period of time, the body develops chronic inflammation, which itself can eventually lead to disease conditions, including allergies, skin problems, and some cancers. Inflammation can also affect organs in so-called autoimmune diseases, in which the immune system attacks its own tissues as if they are threats to health. Examples of some autoimmune chronic inflammatory conditions include inflammation of the heart (myocarditis), kidney (nephritis), large intestine (colitis), and joints (rheumatoid arthritis).
Diagnosis of acute or chronic inflammation involves blood examination to evaluate the increased level of several inflammatory biomarker molecules including gamma globulins, C-reactive protein and fibrinogen. Additionally, patients with chronic conditions would have additional biomarkers assessed, including pro-inflammatory cell-to-cell signalling cytokines, such as tumour necrosis factor alfa (TNF alfa), interleukin-1 beta (IL-1beta), interleukin-6 (IL-6) and interleukin-8 (IL-8). In several research studies, up or down regulation of the expression level of several pro and anti-inflammatory transcription factors have also been assayed. Recently, the possibility of detecting salivary cytokines was assayed in several randomized controlled trails (RCTs), which provided promising results on non-invasive sampling among yoga practitioners even during practice (before and after breathing exercises, for instance).
There are several lifestyle-related risk factors associated with the development of chronic inflammation, such as obesity, unhealthy diet, smoking, stress, and sleep disorders. Altogether these factors induce accumulation of chemically aggressive free radical molecules, an increase in visceral body fat, and higher production of pro-inflammatory cytokines. There are several conventional drugs currently available to treat both acute and chronic inflammatory conditions and/or reduce accompanied symptoms. Depending on the type and severity of symptoms, patients might be prescribed non-steroidal anti-inflammatory drugs (NSAIDs), such as naproxen, ibuprofen, aspirin, acetaminophens (paracetamol), and Tylenol (even though these only reduce pain without affecting the inflammation itself). In more severe cases corticosteroids, disease-modifying antirheumatic drugs (DMARDS), and biological response modifiers (BRMs) might be administered. Anti-inflammatory treatments are prevalent in all known schools of traditional medicine, such as Ayurveda, Chinese medicine, and Russian herbal medicine. Known remedies include a root known as devils claw, the wood spider or grapple plant (Harpagophytum procumnens), the Hyssop plant, ginger, turmeric, and, in some cultures, cannabis.
Behavioural strategies, including lifestyle and dietary changes and mind-body practices, provide another useful tool for treating inflammation. Recent reviews have summarized the research on the benefits of mind-body interventions (MBIs) such as yoga for reducing inflammation in acute and chronic conditions. Even though it is not completely clear how MBIs work at the molecular or cellular level, several hypotheses have been proposed based on recent research advances. First, it has been shown that MBIs reduce expression of gene activity involved in the inflammatory response that are induced by stress. Several studies indicate that these practices are associated with downregulation of the nuclear factor kappa B (NF-kB) pathway, reduced signalling through the proinflammatory transcription factor NF-jB, increased activity of the cAMP response element-binding protein (CREB) family transcription factors, and upregulation of the glucocorticoid receptor gene. Potential mechanisms for these effects include alterations in neuroendocrine, neural, psychological, and behavioural processes. Second, yoga breathing exercises and meditation have been demonstrated to reduce pro-inflammatory cytokines, such as IL-1 beta, IL-6 and TNF-alfa and have a positive impact on depression, anxiety, cognition, and pain. Lastly, yoga and other practices are well known to directly stimulate the vagus nerve. It was found that an increase in vagal tone is correlated with the capacity to regulate the stress response and likely contribute to resilience and the mitigation of mood and anxiety symptoms, which ultimately might reduce inflammation symptoms.
A significant number of RCTs have been conducted to address possible benefits of MBIs on inflammation status of both healthy and diseased individuals. A positive effect of a yoga-based lifestyle intervention was demonstrated in RCTs on groups of healthy individuals exposed to occupational hazards by three independent groups of researchers in India. There was only slight induction of pro-inflammatory factors observed after 12 weeks of regular yoga training as compared with a control group of non-yoga practitioners, in which the induction of proinflammatory factors was significantly higher. This suggests that regular practice of yoga can protect against inflammatory diseases and metabolic risk factors.
Another example of the prophylactic role of yoga is from studies on metabolic syndrome (MetS), which is a well-known precondition associated with diabetes and cardiovascular diseases, defined by increased blood pressure, high blood sugar, excess body weight, and an increased level of numerous biochemical proinflammatory factors. In several recent RCTs conducted independently in Hong Kong and India, it was shown that MetS symptoms were decreased after 12 weeks of regular yoga practices in the study in India and after one year in Hong Kong. In India, healthier choices in diet (dietary interventions) were also included in the intervention. In both cases, it was concluded that yoga and dietary interventions may have an important role in prevention of inflammatory conditions.
In the case of already developed pathologies, yoga might help to reduce post-treatment inflammation conditions and thereby expedite the healing process. In two independent yoga studies on breast cancer survivors (at Ohio State University (OSU) and the University of California, Los Angeles (UCLA)), it was reported that there was reduced activity of NF-kB, increased anti-inflammatory transcription factors, increased proinflammatory cytokines and also improvements in symptoms such as persistent fatigue and vitality in the group assigned to 12 weeks of 90-minute twice weekly hatha (OSU) or Iyengar (UCLA) restorative yoga classes, as compared with the control group. Such improvements are valuable for this population, since cancer survivors are known to be more than twice as likely as individuals without a cancer history to have these symptoms associated with poor health and disability.
Another example of yoga-based complementary/adjunct therapy is research on patients with rheumatoid arthritis (RA), which is a severe chronic inflammatory system disease affecting both psychological and physical health. Comorbid depression is an important psychosomatic factor in this condition, which negatively interferes with the process of recovery. In a recent study from the prestigious All India Institute of Medical Sciences in New Delhi comparing yoga plus RA medication versus RA medications only, the addition of yoga practice to conventional RA treatment re-established immunological tolerance, shown at the molecular and cellular level, along with a significant reduction in depression score. Significant improvements were observed in RA patients after just eight weeks of yoga practice that included, exercises, breathing, and meditation practices as compared with a control group.
In summary, there is an increasing body of research evidence on the positive effect of yoga, other mind-body practices, yogic healthy lifestyle and diet on inflammatory conditions. Long-term yoga and meditation practitioners have been shown to exhibit stronger immediate gene expression changes as compared to short-term practitioners, which in turn evokes the downstream health benefits. However, the “Achilles’s heel” of any behavioural approach is its need for discipline, commitment, and active participation from the patient, in contrast with much of conventional allopathic medicine where drugs and treatments are usually administered to the patient. In this respect, the role of patient self-care and behavioural strategies is very important for success in addressing the widespread occurrence of inflammation and inflammatory conditions.

Naila Omar Khayyam Alieva (Raj Kaur), PhD, is yogi and scientist. She is a certified Kundalini yoga instructor and Gong sound therapy practitioner. Naila teaches Kundalini Yoga and organizes yoga events and workshops in Singapore. She is also an active research scientist at the Institute of Molecular and Cell Biology, A*STAR, Singapore.
Sat Bir Singh Khalsa, Ph.D. is the KRI Director of Research, Research Director for the Kripalu Center for Yoga & Health, and Assistant Professor of Medicine at Harvard Medical School. He has practiced a Kundalini Yoga lifestyle since 1973 and is a KRI certified Kundalini Yoga instructor. He has conducted research on yoga for insomnia, stress, anxiety disorders, and yoga in public schools. He is editor in chief of the International Journal of Yoga Therapy and The Principles and Practice of Yoga in Health Care and author of the Harvard Medical School ebook Your Brain on Yoga.

KRI is a non-profit organization that holds the teachings of Yogi Bhajan and provides accessible and relevant resources to teachers and students of Kundalini Yoga.
More Related Blogs